Diabetes & Me - Sophie Clark
16 Jun 2021 @ 11:29
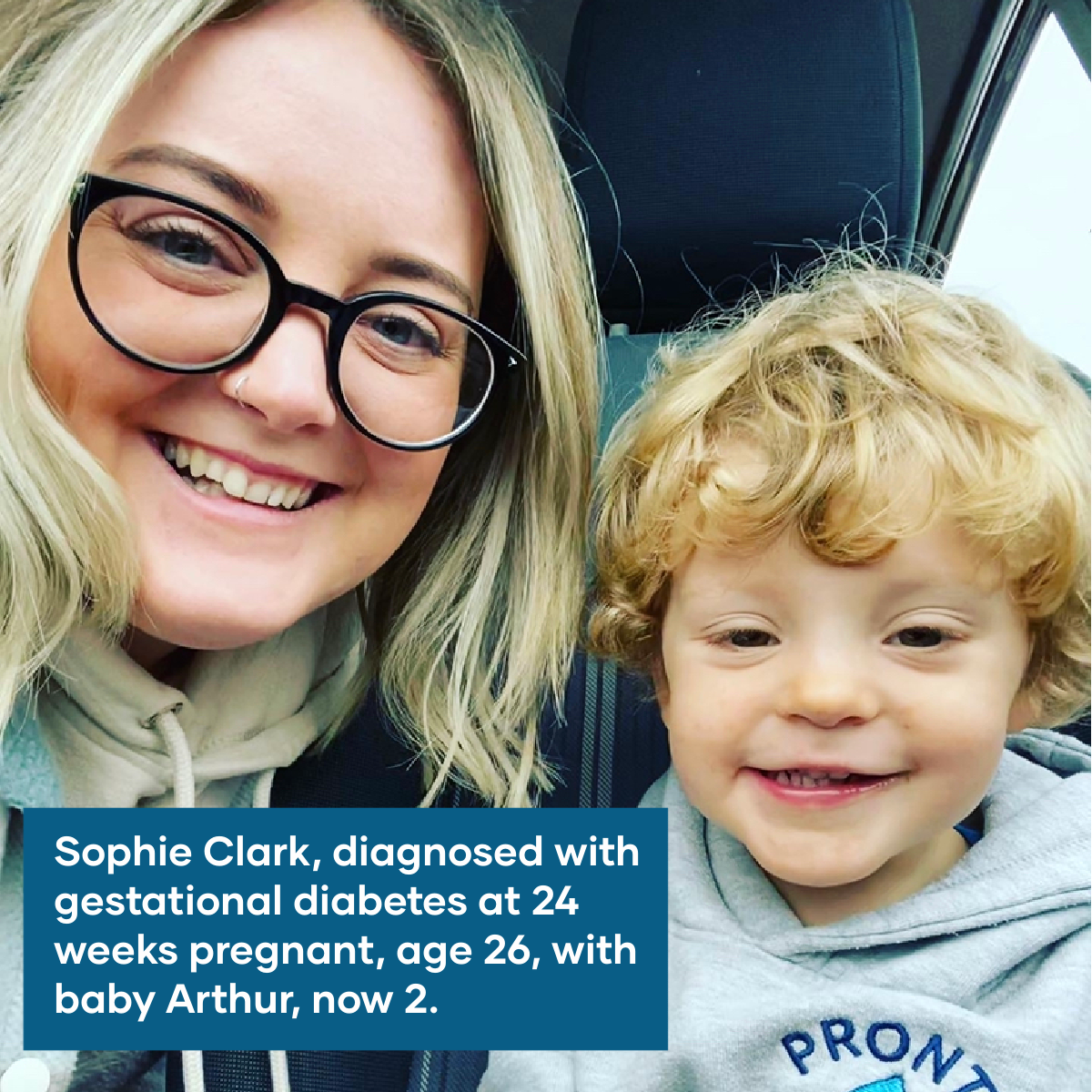
Today's 'Diabetes & Me' feature is with Sophie Clark.
Sophie was diagnosed with gestational diabetes at a routine pregnancy check whilst 24 weeks pregnant.
Gestational diabetes is a type of diabetes that can develop during pregnancy. It affects women who haven't been affected by diabetes before, and usually goes away again after giving birth.
According to statistics from the Diabetes Centre at Noble's, around 75-80 women are diagnosed with gestational diabetes on the island annually.
Here we learn a bit more about Sophie's journey with gestational diabetes.
-------
At what stage in your pregnancy were you diagnosed with gestational diabetes (GD) and how old were you?
I was approximately 24 weeks pregnant when I was diagnosed, and I was 26 years old.
How did they diagnose you?
I had to fast for a minimum of 10 hours (water only) and then my bloods were taken. I was then given a glucose drink and was instructed not to leave the hospital, but to go and find somewhere comfortable to sit for 2 hours. I was still not allowed anything to eat or drink at this point.
Once my 2 hours were up, bloods were taken again to see how my body handled all the extra glucose and I was free to leave.
I received a phone call the next day from a nurse at the Diabetes Centre advising me that I had GD and made an appointment to be seen the same week.
Did you have any symptoms that you were aware of?
I had absolutely no symptoms that I was aware of. We’d just bought and moved into a new house and we’d come back from a trip to Venice so naturally, I was more tired than usual. That being said, I’m sure every pregnant woman would agree that this is normal practice when you’re growing a human, as well as needing to pee more often...
Had you heard of gestational diabetes before you were diagnosed?
I’d never heard of GD until I was at my booking in appointment with the midwife. I didn’t really think much of it at the time either, just that it was a routine part of the pregnancy screening process. My 12 & 20 week scans had gone well and there was nothing to indicate that anything might be out of the ordinary.
How did being diagnosed make you feel at the time?
I was really shocked and upset when I received the phone call to tell me I had gestational diabetes and I rang my partner in floods of tears.
I felt really guilty, that it was my fault and something that I’d done had caused it to happen. I didn’t really know what to expect.
What was the treatment plan for it?
I was booked into the Diabetes Centre clinic where I was seen by a lovely nurse who explained everything to me in much more detail. It was all so overwhelming and again, I burst into tears. She did a great job of reassuring me that it was nothing I’d done and that it was purely a hormonal response to pregnancy and that my body couldn’t keep up with the demands from baby & I.
She gave me a blood glucose testing kit and showed me how to prick my finger and read my blood sugar levels.
I was sent on my way and was given a little book where I had to record my bloods throughout the day when waking up, before and after each meal and then again before bed.
I recorded everything for a week and then went back for a review. Unfortunately, my bloods were not behaving themselves and I was told I would need to start taking tablets and insulin injections too (cue more tears).
I was not prescribed the Freestyle Libre as it wasn’t available at the time, however after doing my homework, this would have saved so many tears and anxiety surrounding the constant injections and finger pricks.
I was also talked through the symptoms of hypers and hypos (when your blood sugar levels are too high or too low) and what to look out for.
I was then shown how to administer the injections and told that I’d now have to check & record my bloods before and after eating, alongside injecting insulin after waking up, before I ate anything and again before bedtime.
Leaving the house with my ‘betes bag containing my finger pricking kit, insulin pens, needle tips and a few packets of Fruit Pastilles in case of emergency quickly became my new normal.
I was seen at the diabetes clinic every other week to review my bloods and was also seen once a month by a consultant to see how things were progressing pregnancy wise.
I was also given regular scans to monitor the baby’s growth as I was told I’d ‘probably have a big baby’.
Did your diagnosis have any effect on your birth plans?
I didn’t have a birth ‘plan’ as such to begin with, more of a birth ‘preference’ as the reality is, things don’t always go to plan, and I didn’t want to have my heart set on something and feel disappointed if it went in another direction.
I was told that I wouldn’t be allowed to carry past 38 weeks due to the increased risk of complications.
I was also told quite matter of factly by the consultant that there was a higher chance of having a stillborn baby which naturally, absolutely terrified us as parents.
I was asked how I felt about being booked in for a c-section but I was quite adamant that I wanted to at least try for a vaginal birth, so it was agreed that I would be induced and I was given a date that this would happen.
Was everything ok with you and Arthur once he was born?
At around 36 weeks I’d noticed a reduction in his movements/kicks and I noticed that my blood sugar levels were dropping quite quickly and I ended up having a few hypos in this period too.
After being monitored for around 3/4 days I was eventually sent for another growth scan to check on the progress. This scan showed that he had stopped growing and I was told that I would need to induced straight away to avoid any further complications.
Apart from monitoring the baby constantly and my partner pricking my finger every half hour or so to check my bloods were okay (cue Nurse Dale) I had a very straight forward labour.
Arthur was born at 37 weeks and that ‘big baby’ I was told I’d be having actually only ended up being 5lb 11oz.
It turns out that the insulin I had been injecting to keep us both safe had actually caused the placenta to deteriorate, his cord was also around his neck, so he wasn’t getting everything he needed and was struggling.
We were very lucky that Arthur didn’t need to be taken to SCBU but the midwives did keep a close eye on him and performed heel prick blood tests regularly to ensure his bloods were okay, he also had some jaundice.
Apart from that, he was absolutely fine and we were allowed home 2 days later.
Did the treatment for diabetes continue following the birth?
Once I’d delivered Arthur I was told the diabetes would disappear. I was told to stop all medication but asked to continue to monitor my blood sugar levels for the next 24/48 hours just to be on the safe side.
I was asked to attend the Diabetes Centre around 12 weeks post-delivery to ensure that I hadn’t developed type 2 diabetes. Arthur is 3 at the end of this month and I’m pleased to say that this has had no lasting effect on either of us, however there is an increased chance that i'll develop GD again in any future pregnancies.
Any words of advice/wisdom for other mums recently diagnosed with gestational?
Please do not blame yourself and stay away from Dr. Google!
I found that there were lots of Facebook groups for mums in the same situation which helped knowing that I wasn’t alone.
I would also highlight the important of monitoring your baby’s movements. If something doesn’t feel right, please contact the Jane. No matter how many times you might have to go in and out, you’re not being a nuisance and it’s just not worth taking the risk.
It’s so, so important and something I bang on about all the time to my friends who are expecting. You can visit https://www.kickscount.org.uk for more info.
Last but not least, pack a big bar of chocolate in your hospital bag for post delivery (you absolutely deserve it).
-------
Diabetes affects around 6% of the island’s population, and that is set to increase. The signs and symptoms of diabetes can develop at any time, and early diagnosis is so important to help prevent further health complications.
If you or someone you know is experiencing any of the following symptoms, get in touch with your GP: going to the toilet a lot, especially at night; excessive thirst; feeling more tired than usual; losing weight without trying to; genital itching or thrush; cuts and wounds take longer to heal; and blurred vision.
